Clinical and Molecular Hematology
Contatti
Settore ERC
Attività
Research activity
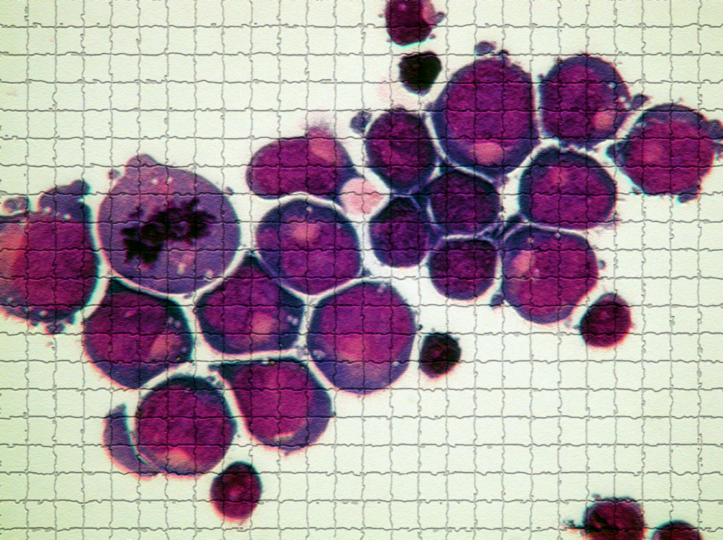
The Clinical and Molecular Hematology Unit directed by Prof. Cilloni is composed of biologists/biotechnologists and clinicians who deal with the understanding of the molecular basis of onco-haematological diseases. The main research interests of the Clinical and Molecular Hematology division are the study of the role of oncogenic and tumor suppressor genes in the pathogenesis and progression of hematological neoplasms, the identification and clinical validation of diagnostic and prognostic biomarkers, the study of mitochondrial metabolism in myelodysplastic and iron overload syndromes, and the development of innovative diagnostic/prognostic assays.
Ongoing Projects
IDH2 mutations hunter – I.M.HU
Settore: MED/15 – Malattie del sangue; MED/46 – Scienze tecniche di medicina di laboratorio; BIO/12 – Biochimica clinica e biologia molecolare clinica
Ente finanziatore: Call for the implementation of patent enhancement programs through the financing of Proof of Concept (PoC) projects - TOINPROVE / 2020, issued by MISE
Participants to the project: The research group at Dept. Clinical and Biological Sciences (DSCB) includes Prof. Daniela Cilloni (Full Professor, Principal Investigator); Prof. Carmen Fava (Associate Professor); Prof. Marco Lo Iacono (Associate Professor); Dr. Petiti Jessica (Research Fellow).
The team at DSCB for this project collaborates with Mrs. Francesca Caciolli (Resident in Internal Medicine, Department of Medical Sciences, University of Turin) and other 7 Italian diagnostic laboratories.
Abstract: The Isocitrate dehydrogenase 2 (IDH2) gene is an enzyme that catalyzes the first reaction of oxidative decarboxylation in the Krebs cycle. Mutations in this gene have been observed in various pathologies including acute myeloid leukemia (AML) and myelodysplasias (MDS). The most frequent mutations of IDH2 in AML and MDS, affecting more than 95% of mutated patients, involve the arginine residues in positions R140 and R172. IDH2 is considered a molecular marker for diagnosis and minimal residual disease, especially in the absence of other alterations. In addition, a specific drug has recently been approved for IDH2 mutations. For these reasons, it is essential to monitor the status of IDH2. Currently, to evaluate the IDH2 status in these patients, Sanger sequencing and the droplet digital PCR (ddPCR) are considered valid approaches. Sanger sequencing is the most used method but is negatively characterized by its high detection limit (~ 20%); on the contrary, ddPCR is a highly sensitive and accurate technology, but still not widespread. Both methods have the disadvantage of being laborious and needing expensive specific equipment and reagents.
In the present project, we intend to develop a prototype of a PNA-PCR Clamping-based diagnostic kit, able to identify the most frequent IDH2 mutations: R140 and R172, observed in 74.8% and 20.4% of mutated IDH2 cases, respectively. This kit will make the diagnosis faster, cheaper, and it is more sensitive than Sanger sequencing, allowing the molecular characterization of IDH2 in any laboratory.
Scientific Publications related to the project
- Rosso V, Petiti J, Dragani M, Andreani G, Croce E, Lo Iacono M, Saglio G,Fava C, Cilloni D. Clone wars: co-occurrence of IDH2 R140Q and R172K in myelodysplastic syndromes. Ann Hematol. 2020 Apr;99(4):891-893. doi: 10.1007/s00277-020-03913-x. Epub 2020 Feb 4. PMID: 32016578.
- Petiti J, Rosso V, Croce E, Franceschi V, Andreani G, Dragani M, De Gobbi M, Lunghi M, Saglio G, Fava C, Lo Iacono M, Cilloni D. Highly Sensitive Detection of IDH2 Mutations in Acute Myeloid Leukemia. J Clin Med. 2020 Jan 19;9(1):271. doi: 10.3390/jcm9010271. PMID: 31963812; PMCID: PMC7019902.
- Petiti J, Rosso V, Lo Iacono M, Calabrese C, Signorino E, Gaidano V, Berger M, Saglio G, Cilloni D. Prognostic significance of The Wilms' Tumor-1 (WT1) rs16754 polymorphism in acute myeloid leukemia. Leuk Res. 2018 Apr;67:6-11. doi: 10.1016/j.leukres.2018.01.016. Epub 2018 Feb 5. PMID: 29407184.
- Rosso V, Petiti J, Bracco E, Pedrola R, Carnuccio F, Signorino E, Carturan S, Calabrese C, Bot-Sartor G, Ronconi M, Serra A, Saglio G, Frassoni F, Cilloni D. A novel assay to detect calreticulin mutations in myeloproliferative neoplasms. 2017 Jan 24;8(4):6399-6405. doi: 10.18632/oncotarget.14113. PMID: 28031530; PMCID: PMC5351640.
- Rosso V, Bracco E, Pedrola R, Carturan S, Signorino E, Petiti J, Calabrese C, Nicoli P, De Gobbi M, Gaidano V, Gallo D, Ulisciani S, Fava C, Rege-Cambrin G, Frassoni F, Saglio G, Cilloni D. Detection of BCR-ABL T315I mutation by peptide nucleic acid directed PCR clamping and by peptide nucleic acid FISH. Biomark Res. 2015 Jul 3;3:15. doi: 10.1186/s40364-015-0039-y. PMID: 26146560; PMCID:
Patient-specific FLT3 ITD evaluation
Settore: MED/15 – Malattie del sangue; MED/46 – Scienze tecniche di medicina di laboratorio; BIO/12 – Biochimica clinica e biologia molecolare clinica
Ente finanziatore: Astellas Pharma
Participants to the project: The research group at Dept. Clinical and Biological Sciences (DSCB) includes Prof. Daniela Cilloni (Full Professor, Principal Investigator); Prof. Carmen Fava (Associate Professor); Dr. Petiti Jessica (Research Fellow); Mrs. Valentina Bonuomo (PhD Student).
Abstract: FLT3 mutations are present in around 35% of AML patients. FLT3- ITD mutations with high allele ratio have been associated with inferior prognosis. Several FLT3 inhibitors have been evaluated in clinical trials. The prognostic significance of MRD positivity after chemotherapy or before hematopoietic stem cell transplantation has been largely demonstrated. Despite of this, FLT3 ITD is not used as marker of MRD. The detection of these small clones is correlated with the sensitivity of the method. Few years ago, Zuffa et al. analyzed retrospectively 5 patients who relapsed as FLT3 ITD positive by ultra-deep sequencing (UDS) and they found that these patients carried a small FLT3 ITD+ clone at diagnosis, which was undetectable by routine analysis. In the last years, the evaluation of MRD after stem cell transplantation has become a routine approach to predict imminent relapse and to implement prevention strategies. The possibility of early identify small clones offers the possibility of treatment with powerful inhibitors such as gilteritinib.
Setting up a droplet digital PCR using patient-specific primers and probes for FLT3 ITD, we intend i) to investigate the prognostic role of small FLT3-ITD+ clones detectable only with a highly sensitive, precise and “personalized” method; ii) to identify the factors that might have an impact in the selection of clones; iii) to clarify the value of FLT3 as a marker of MRD during chemotherapy and before and after stem cell transplantation and iv) to verify whether FLT3 inhibitors can completely eradicate the FLT3 mutated clone.
Scientific Publications related to the project
- Petiti J, Lo Iacono M, Dragani M, Pironi L, Fantino C, Rapanotti MC, Quarantelli F, Izzo B, Divona M, Rege-Cambrin G, Saglio G, Gottardi EM, Cilloni D, Fava C. Novel Multiplex Droplet Digital PCR Assays to Monitor Minimal Residual Disease in Chronic Myeloid Leukemia Patients Showing Atypical BCR-ABL1 Transcripts. J Clin Med. 2020 May 13;9(5):1457. doi:10.3390/jcm9051457. PMID: 32414125; PMCID: PMC7290999.
- Cilloni D, Petiti J, Rosso V, Andreani G, Dragani M, Fava C, Saglio G. Digital PCR in Myeloid Malignancies: Ready to Replace Quantitative PCR? Int J Mol Sci. 2019 May 7;20(9):2249. doi: 10.3390/ijms20092249. PMID: 31067725; PMCID: PMC6540058.
- Andreani G, Cilloni D. Strategies for minimal residual disease detection: current perspectives. Blood Lymphat Cancer. 2019 Feb 12;9:1-8. doi:10.2147/BLCTT.S172693. PMID: 31807111; PMCID: PMC6855617.
- Willemze R, Suciu S, Meloni G, Labar B, Marie JP, Halkes CJ, Muus P, Mistrik M, Amadori S, Specchia G, Fabbiano F, Nobile F, Sborgia M, Camera A, Selleslag DL, Lefrère F Sr, Magro D, Sica S, Cantore N, Beksac M, Berneman Z, Thomas X, Melillo L, Guimaraes JE, Leoni P, Luppi M, Mitra ME, Bron D, Fillet G, Marijt EW, Venditti A, Hagemeijer A, Mancini M, Jansen J, Cilloni D, Meert L, Fazi P, Vignetti M, Trisolini SM, Mandelli F, de Witte T. High-dose cytarabine in induction treatment improves the outcome of adult patients younger than age 46 years with acute myeloid leukemia: results of the EORTC-GIMEMA AML-12 trial. J Clin Oncol. 2014 Jan 20;32(3):219-28. doi: 10.1200/JCO.2013.51.8571. Epub 2013 Dc 2. PMID: 24297940.
- Lo-Coco F, Cuneo A, Pane F, Cilloni D, Diverio D, Mancini M, Testoni N, Bardi A, Izzo B, Bolli N, La Starza R, Fazi P, Iacobelli S, Piciocchi A, Vignetti M, Amadori S, Mandelli F, Pelicci PG, Mecucci C, Falini B, Saglio G; Acute Leukemia Working Party of the GIMEMA group. Prognostic impact of genetic characterization in the GIMEMA LAM99P multicenter study for newly diagnosed acute myeloid leukemia. 2008 Jul;93(7):1017-24. doi: 10.3324/haematol.12004. Epub 2008 May 27. PMID: 18508799.
Role of c-Src kinase in the regulation of Bcl-x splicing in myeloproliferative diseases
Settore: MED/15 – Malattie del sangue; BIO/11 – Biologia molecolare; BIO/13 – Biologia applicata
Participants to the project: The research group at Dept. Clinical and Biological Sciences (DSCB) includes Prof. Daniela Cilloni (Full Professor, Principal Investigator); and Dr. Petiti Jessica (Research Fellow) and Dr. Veronica Sciannameo (Research Fellow).
The team at DSCB for this project collaborates with Dr. Marco Armenio, MD (Specialist in Hematology, Mauriziano Hospital) and Mr. Federico Itri (Resident in Internal Medicine, Department of Medical Sciences, University of Turin)
Abstract: Myeloproliferative neoplasms are divided into essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF). Although ruxolitinib was proven to be effective in reducing symptoms, patients rarely achieve complete molecular remission. Bcl-xL protein, the long isoform encoded by alternative splicing of the Bcl-x gene, acts as an anti-apoptotic regulator. We found that Bcl-xL is progressively over-expressed in cells from ET, PV, and PMF patients, independently by JAK2 mutational status. Moreover, the combination of ABT-737, a Bcl-xL inhibitor, and ruxolitinib resulted in a significantly higher apoptotic rate than the individual drug, demonstrating that targeting simultaneously JAK2 and Bcl-xL might represent an interesting new therapeutical approach. Since ABT-737 is characterized by poor bioavailability, new approaches to target Bcl-xL must be explored. This project aims to investigate the pathway of the SRC family in MPNs, particularly the role played by SRC kinases in modulating Bcl-x splicing through Sam68 and hnRNPA1. A better comprehension of this mechanism could help us to indirectly target Bcl-xL, opening a new frontier in MPNs treatment.
Scientific Publications related to the project
- Guglielmelli P, Palandri F, Selleri C, Cilloni D, Mendicino F, Mazza P, Pastore D, Palumbo GA, Santoro M, Pavone V, Impera S, Morelli M, Coco P, Valsecchi D, Passamonti F, Breccia M; ROMEI study group. Adherence to ruxolitinib, an oral JAK1/2 inhibitor, in patients with myelofibrosis: interim analysis from an Italian, prospective cohort study (ROMEI). Leuk Lymphoma. 2022 Jan;63(1):189-198. doi:10.1080/10428194.2021.1969388. Epub 2021 Sep 15. PMID:34521299.
- Petiti J, Lo Iacono M, Rosso V, Andreani G, Jovanovski A, Podestà M, Lame D, Gobbi M, Fava C, Saglio G, Frassoni F, Cilloni D. Bcl-xL represents a therapeutic target in Philadelphia negative myeloproliferative neoplasms. J Cell Mol Med. 2020 Sep;24(18):10978-10986. doi: 10.1111/jcmm.15730. Epub 2020 Aug 13. PMID: 32790151; PMCID: PMC7521327.
- Crisà E, Cilloni D, Elli EM, Martinelli V, Palumbo GA, Pugliese N, Beggiato E, Frairia C, Cerrano M, Lanzarone G, Marchetti M, Mezzabotta M, Boccadoro M, Ferrero D. The use of erythropoiesis-stimulating agents is safe and effective in the management of anaemia in myelofibrosis patients treated with ruxolitinib. Br J Haematol. 2018 Sep;182(5):701-704. doi: 10.1111/bjh.15450. Epub 2018 Jul 9. PMID: 29984826.
Research activity
The Clinical Unit “Internal Medicine with hematological focus” is located at the AOU San Luigi, Orbassano (TO) and is part of the Department of Clinical and Biological Science since 1998. It includes a clinical-nursing team and collaborates with translational and "basic" research groups, sharing the common interest in understanding the molecular basis of onco-haematological diseases and how this knowledge can be quickly translated into better clinical care. The clinical and scientific work is closely integrated with the SCDU "Hematology" of the AO Ordine Mauriziano of Turin.
The clinical infrastructures for the treatment of patients suffering from haematological diseases include an ordinary hospitalization area with 9 beds, an intensive hospitalization area with 8 beds with low bacterial load (4 of which reserved for transplantation activities) and an Out-patient/Day Hospital Unit.
The infrastructures comprise also a molecular diagnostic facility (member of the Italian Consortium LabNet) specializing in molecular and cytogenetic testing for acute leukemia, myelodysplastic syndromes, myeloproliferative neoplasms, thalassemia and hemochromatosis, and basic research laboratories furnished with all the main apparatus for advanced molecular and cellular analyses.
The primary research interests are:
- Molecular biology of haematological malignancies
- Hematopoietic stem cell transplantation
- Participation to intervantional clinical trials on new pharmaceutical approaches for hematological neoplasms
- Participation to observational studies in onco-hematology and hematopoietic stem cell transplantation fields
Ongoing projects
Breve descrizione divulgativa dei principali progetti di ricerca del gruppo, avendo cura di sottolinearne razionale e obiettivi.
Autologous Hematopoietic Stem Cell Transplantation in Multiple Sclerosis Patients
Settore: MED/09, MED/15, MED/26
Ente finanziatore: None
Partecipanti al progetto: Marco De Gobbi, Collaborators: Marco Capobianco
Abstract: Autologous hematopoietic stem cell transplantation (AHSCT) has been used in the treatment of highly active multiple sclerosis (MS) for over two decades. It has been demonstrated to be highly efficacious in relapsing-remitting (RR) MS patients failing to respond to disease-modifying drugs (DMDs). AHSCT guarantees higher rates of no evidence of disease activity (NEDA) than those achieved with any other DMDs, but it is also associated with greater short-term risks which have limited its use. In the 2019 updated EBMT and ASBMT guidelines, which review the clinical evidence of AHSCT in MS, AHSCT indication for highly active RRMS has changed from "clinical option" to "standard of care". On this basis, AHSCT must be proposed on equal footing with second-line DMDs to patients with highly active RRMS, instead of being considered as a last resort after failure of all available treatments. The decision-making process requires a close collaboration between transplant hematologists and neurologists and a full discussion of risk-benefit of AHSCT and alternative treatments.
Pubblicazioni
- Bertolotto A, Martire S, Mirabile L, Capobianco M, De Gobbi M, Cilloni D. Autologous Hematopoietic Stem Cell Transplantation (AHSCT): Standard of Care for Relapsing-Remitting Multiple Sclerosis Patients. Neurol Ther. 2020 Dec;9(2):197-203. doi: 10.1007/s40120-020-00200-9. Epub 2020 Jun 16
- Boffa G, Massacesi L, Inglese M, Mariottini A, Capobianco M, Lucia M, Amato MP, Cottone S, Gualandi F, De Gobbi M, Greco R, Scimè R, Frau J, Zimatore GB, Bertolotto A, Comi G, Uccelli A, Signori A, Angelucci E, Innocenti C, Ciceri F, Repice AM, Sormani MP, Saccardi R, Mancardi G; Italian BMT-MS study group. Long-Term Clinical Outcomes of Hematopoietic Stem Cell Transplantation in Multiple Sclerosis. Neurology. 2021 Jan 20:10.1212/WNL.0000000000011461. doi: 10.1212/WNL.0000000000011461. Online ahead of print
Implications of Thio-metabolome Graft versus Host Disease after allogeneic hematopoietic stem cell transplantation
Settore: MED/09, MED/15, BIO/14
Partecipanti al progetto: Marco De Gobbi, Collaborators: Silvia De Francia, Sarah Allegra, Francesco Chiara
Abstract: The Glutathione (GSH) is a tripeptide (γ-Glu-Cys-Gly) with independent ribosomal biosynthesis. The γ-glutamyl cycle contains the metabolic pathway of GSH synthesis and degradation. Three of the six reactions of γ-glutamyl cycle are linked with other metabolic pathways (EMP, TCA cycle, methylglyoxal). At systemic level, these metabolic pathways are fundamental to understand pathogenic mechanism. Experimental evidence shows a strong correlation between GSH-dependent metabolism and the survival of cancer cells subjected to apoptotic signal or oxidative stress. Besides there is evidence that graft versus host disease (GvHD), a complication of allogeneic hemathopoietic stem cells transplantation (HSCT) has a direct correlation with plasma levels of cysteine/cystine in conjunction with a redox imbalance with altered levels of GSH/GSSG with up-regulation of inflammatory cytokines. The potential therapeutic evaluation of GSH may be of real clinical interest for HSCT patients with GvHD.
Primary objective: find prognostic and diagnostic biomarker for clinical monitoring GvDH post HSCT patients. The evidence of metabolomic study can determine an impactful on clinical therapeutic protocol for GvDH treatment. The intracellular metabolism of cell-type involved in hemato-oncological diseases is actually unresearched.
Secondary objective: internal validation of the analytical methods implemented during the study and analytical study of the biochemical evidence obtained, currently not found with traditional routine techniques, by means of validated original methodologies.
Definition of biological mechanisms related to Luspatercept therapy
Settore: MED/09, MED/15, MED/03, MED/38, BIO/14, BIO/17
Partecipanti al progetto: Marco De Gobbi, Federico Itri. Collaborators: Giovanni Battista Ferrero, Antonella Roetto, Antonio D’Avolio, Enzo Medico
Abstract: Luspatercept is a recombinant fusion protein which, acting as a ligand trap, attenuates the interaction of some ligands of the transforming growth factor beta (TGF-β) family with receptors located on erythroblasts, allowing their maturation, reducing ineffective erythropoiesis, and thus increasing hemoglobin levels. It has not been definitively clarified what are the molecular mechanisms involved in the pharmacological effect of this protein. In particular, the ligands that mediate the effect of Luspatercept and what are the effects of their pharmacologically induced inhibition on the metabolism of erythroblasts have not been definitively identified. Furthermore, the effect of this treatment on martial homeostasis is not yet defined.
Therapy with Luspatercept allowed the restoration of erythroblast maturation in β-thalassemia and also in low-risk myelodysplastic syndromes (MDS), clonal bone marrow disorders characterized by hematopoiesis (in particular erythropoiesis) dysplastic and ineffective. In this context, Luspatercept can be prescribed in patients with myelodysplasia with ring sideroblasts (MDS-RS). Clinical trials are also underway to evaluate the efficacy of Luspatercept also in other low-risk MDSs.
The aim of the study is to better characterize and understand the response to Luspatercept in β-thalassemia and low-risk MDS analysing the indices of erythropoiesis and martial homeostasis β-thalassemia and MDS patients on standard therapy with or without Luspatercept. Among these indices, some molecules recently identified as possible markers of ineffective erythropoiesis (GDF11, GDF15) and hormones involved in martial homeostasis (hepcidin, erythroferron) will be studied. Furthermore, the transcription profile of circulating erythroid cells will be analyzed in a subgroup of patients by RNA sequencing.
Research activity
Prof. Fava's research group is made up of clinicians, biologists and medical statisticians. The research activity concerns chronic myeloproliferative neoplasms and consists in a better understanding of the pathogenesis of the diseases, of the factors that determine their progression and in the identification of new prognostic factors.
Furthermore, part of the research is dedicated to the validation of new, more sensitive and accurate diagnostic methods for the evaluation of minimal residual disease in the context of Philadelphia positive leukemias.
Ongoing Projects
Standardization of BCR-ABL p190 molecular analysis
Settore: MED/15, MED/01
Ente finanziatore: Compagnia San Paolo
Partecipanti al progetto: Prof. Carmen Fava (Assistant Professor), Prof Paola Berchialla (Assistant Professor), Dr Jessica Petiti (Research Fellow)
Abstract: Acute lymphoblastic leukemia (ALL) occurs at any age, progresses rapidly and is fatal within months if untreated. In ALL, a chromosomal abnormality creates the BCR-ABL1 gene. Monitoring of BCR-ABL1 is a crucial prognostic tool. Molecular analysis of its most frequent variant, p190, has not yet been optimized nor standardized. An Italian consortium for standardization of methods to measure the p190 BCR-ABL1 has been designed to overcome the lack of standardization of laboratory procedures and data interpretation.
However, reference materials for p190 are still missing and comparability of results is unmet. This project aims to produce traceable reference materials for p190 BCR-ABL1 and to develop a methodology to measure ALL during monitoring.
Pubblicazioni
Jovanovski A, Petiti J, Giugliano E, Gottardi EM, Saglio G, Cilloni D, Fava C. Standardization of BCR-ABL1 p210 Monitoring: From Nested to Digital PCR. Cancers (Basel). 2020 Nov 6;12(11):3287. doi: 10.3390/cancers12113287. PMID:33172063; PMCID: PMC7694607.
Italy-TFR: Observational Study in Adult Patients with Chronic Myeloid Leukemia who discontinue Tyrosine Kinase Inhibitors in Italy
Settore: MED/15, MED/01
Ente finanziatore: Associazione Italiana Leucemie
Partecipanti al progetto: Prof. Carmen Fava (Assistant Professor), Prof Paola Berchialla (Assistant Professor), Veronica Sciamanneo (PhD Student)
Abstract: It is judged safe to discontinue treatment with tyrosine kinase inhibitors (TKI) for chronic myeloid leukemia (CML) in experimental trials on treatment-free remission (TFR). We collected a total of 293 Italian patients with chronic phase CML who discontinued TKI in deep molecular response. Seventy-two percent of patients were on treatment with imatinib, and 28% with second generation TKI at the time of discontinuation. Median duration of treatment with the last TKI was 77 months [Interquartile Range (IQR) 54;111], median duration of deep molecular response was 46 months (IQR 31;74). Duration of treatment with TKI and duration of deep molecular response were shorter with second generation TKI than with imatinib (P<0.001). Eighty-eight percent of patients discontinued as per clinical practice, and reasons for stopping treatment were: toxicity (20%), pregnancy (6%), and shared decision between treating physician and patient (62%). After a median follow up of 34 months (range, 12-161) overall estimated TFR was 62% (95%CI: 56;68). At 12 months, TFR was 68% (95%CI: 62;74) for imatinib, 73% (95%CI: 64;83) for second generation TKI. Overall median time to restart treatment was six months (IQR 4;11). No progressions occurred. Although our study has the limitation of a retrospective study, our experience within the Italian population confirms that discontinuation of imatinib and second generation TKI is feasible and safe in clinical practice. On the basis of these previous results we proposed a retrospective and prospective observational study to increase the the population and extend the follow-up, with the purpose of developing and validating predictors of TFR success.
Pubblicazioni
- Fava C, Rege-Cambrin G, Dogliotti I, Cerrano M, Berchialla P, Dragani M, Rosti G, Castagnetti F, Gugliotta G, Martino B, Gambacorti-Passerini C, Abruzzese E, Elena C, Pregno P, Gozzini A, Capodanno I, Bergamaschi M, Crugnola M, Bocchia M, Galimberti S, Rapezzi D, Iurlo A, Cattaneo D, Latagliata R, Breccia M, Cedrone M, Santoro M, Annunziata M, Levato L, Stagno F, Cavazzini F, Sgherza N, Giai V, Luciano L, Russo S, Musto P, Caocci G, Sorà F, Iuliano F, Lunghi F, Specchia G, Pane F, Ferrero D, Baccarani M, Saglio G. Observational study of chronic myeloid leukemia Italian patients who discontinued tyrosine kinase inhibitors in clinical practice. Haematologica. 2019 Aug;104(8):1589-1596. doi: 10.3324/haematol.2018.205054. Epub 2019 Feb 28. PMID: 30819917; PMCID: PMC6669161.
- Dragani M, Rege-Cambrin G, Ferrero D, Abruzzese E, Pregno P, Elena C, Cedrone M, Santoro M, Andreani G, Saglio G, Fava C. Beyond the comfort zone of deep molecular response: discontinuation in major molecular response chronic myeloid leukemia. Leuk Lymphoma. 2019 Dec;60(13):3330-3332. doi: 10.1080/10428194.2019.1622103. Epub 2019 Jun 4. PMID: 31161827.
- Dragani M, Petiti J, Rege-Cambrin G, Gottardi E, Daraio F, Caocci G, Aguzzi C, Crisà E, Andreani G, Caciolli F, Fava C. Treatment-Free Remission in Chronic Myeloid Leukemia Harboring Atypical BCR-ABL1 Transcripts. Mediterr J Hematol Infect Dis. 2020 Sep 1;12(1):e2020066. doi: 10.4084/MJHID.2020.066. PMID:32952977; PMCID: PMC7485467.
- Dragani M, Rege Cambrin G, Berchialla P, Dogliotti I, Rosti G, Castagnetti F, Capodanno I, Martino B, Cerrano M, Ferrero D, Gambacorti-Passerini C, Crugnola M, Elena C, Breccia M, Iurlo A, Cattaneo D, Galimberti S, Gozzini A, Bocchia M, Lunghi F, Cedrone M, Sgherza N, Luciano L, Russo S, Santoro M, Giai V, Caocci G, Levato L, Abruzzese E, Sora F, Saglio G, Fava C. A Retrospective Analysis about Frequency of Monitoring in Italian Chronic Myeloid Leukemia Patients after Discontinuation. J Clin Med. 2020 Nov 17;9(11):3692. doi: 10.3390/jcm9113692. PMID: 33213044; PMCID: PMC7698481.
Evaluation of the prognostic value of digital PCR in patients with chronic myeloid leukemia
Settore: MED/15, MED/01
Ente finanziatore: Fondazione CRT
Partecipanti al progetto: Prof. Carmen Fava (Assistant Professor), Dr Jessica Petiti (Research Fellow), Prof Paola Berchialla (Assistant Professor), Veronica Sciamanneo (PhD Student), Prof. Daniela Cilloni (Full Professor)
Abstract: BCR-ABL1 mRNA levels represent the key molecular marker for the evaluation of minimal residual disease (MRD) in chronic myeloid leukemia (CML) patients and real-time quantitative PCR (RT-qPCR) is currently the standard method to monitor it. In the era of tyrosine kinase inhibitors (TKIs) discontinuation, droplet digital PCR (ddPCR) has emerged to provide a more precise detection of MRD. To hypothesize the use of ddPCR in clinical practice, we designed a multicentric study to evaluate the potential value of ddPCR in the diagnostic routine. Thirty-seven RNA samples from CML patients and five from healthy donors were analyzed using both ddPCR QXDxTMBCR-ABL %IS Kit and LabNet-approved RT-qPCR methodologies in three different Italian laboratories. Our results show that ddPCR has a good agreement with RT-qPCR, but it is more precise to quantify BCR-ABL1 transcript levels. Furthermore, we did not find differences between duplicate or quadruplicate analysis in terms of BCR-ABL1% IS values. Droplet digital PCR could be confidently introduced into the diagnostic routine as a complement to the RT-qPCR. We further expored ddPCR in the setting of patients who discontinued treatment with Tyrosine Kinase Inhibitors and particular we used this method on patients with atypical transcripts.
Pubblicazioni
- Petiti J, Dragani M1, Castelli A, Lo Iacono M1, Fantino C, Badino C, Serra A, Giugliano E, Andreani G, Rosso V, Gottardi E, RegeCambrin G, Saglio G, Cilloni D and Fava C. Characterization and monitoring by droplet digital PCR of a novel BCR-ABL1 fusion transcript in a patient with chronic myeloid leukemia. January 2020. Journal of Translational Science 6(5):2020. DOI:10.15761/JTS.1000369
- Petiti J, Lo Iacono M, Dragani M, Pironi L, Fantino C, Rapanotti MC, Quarantelli F, Izzo B, Divona M, Rege-Cambrin G, Saglio G, Gottardi EM, Cilloni D, Fava C. Novel Multiplex Droplet Digital PCR Assays to Monitor Minimal Residual Disease in Chronic Myeloid Leukemia Patients Showing Atypical BCR-ABL1 Transcripts. J Clin Med. 2020 May 13;9(5):1457. doi:10.3390/jcm9051457. PMID: 32414125; PMCID: PMC7290999.
- Diral E, Mori S, Antolini L, Abruzzese E, Le Coutre P, Martino B, Pungolino E, Elena C, Bergamaschi M, Assouline S, Di Bona E, Gozzini A, Andrade-Campos M, Stagno F, Iurlo A, Pirola A, Fontana D, Petiti J, Bonanomi ML, Crivori P, Piazza R, Fava C, Gambacorti-Passerini C. Increased tumor burden in patients with chronic myeloid leukemia after 36 months of imatinib discontinuation. 2020 Nov 5;136(19):2237-2240. doi: 10.1182/blood.2019004371. PMID: 32518953. IF 22.113; TC Scopus 2; TC WOS 3; BEST TC 3; Q1 Scopus; Q1 WOS
- Fava C, Bernardi S, Gottardi EM, Lorenzatti R, Galeotti L, Ceccherini F, Cordoni F, Daraio F, Giugliano E, Jovanovski A, Petiti J, Varotto M, Barberio D, Rege-Cambrin G, Berchialla P, Sciannameo V, Malagola M, Saglio G, Russo D. Alignment of Qx100/Qx200 Droplet Digital (Bio-Rad) and QuantStudio 3D (Thermofisher) Digital PCR for Quantification of BCR-ABL1 in Ph+ Chronic Myeloid Leukemia. 2021 May 5;9(2):35. doi: 10.3390/diseases9020035.PMID: 34062996.
- Droplet Digital PCR for BCR-ABL1Monitoring in Diagnostic Routine: Ready to Start? Bochicchio MT, Petiti J, Berchialla P, Izzo B, Giugliano E, Ottaviani E, Errichiello S, Rege-Cambrin G, Venturi C, Luciano L, Daraio F, Calistri D, Rosti G, Saglio G, Martinelli G, Pane F, Cilloni D, Gottardi EM, Fava C. Cancers (Basel). 2021 Oct 30;13(21):5470. doi: 10.3390/cancers13215470.PMID: 34771634
Interaction between gut microbiota and tyrosine kinase inhibitors in defining the clinical outcomes of patients with chronic myeloid leukemia
Settore: MED/15, MED/01
Ente finanziatore: Pfizer
Partecipanti al progetto: Prof. Carmen Fava (Assistant Professor), Prof Paola Berchialla (Assistant Professor), Prof. Daniela Cilloni (Full Professor)
Abstract: Philadelphia positive Chronic Myeloid Leukemia (CML) is a myeloproliferative neoplasm that originates from a pluripotent hematopoietic cell. CML treatment is based on tyrosine-kinase inhibitors (TKIs) which have dramatically improved long-term survival rates. Although these drugs are generally well tolerated, TKIs are not free from side effects, especially gastrointestinal such as diarrhea, constipation, abdominal pain, malabsorption, bleeding and increase in liver and pancreatic enzymes, which generally emerge in the first three months of therapy and can persist over time, affecting the quality of life and compliance of the patients. In addition, a higher incidence of time and dose-dependent cardiovascular events (up to 20% in patients with risk factors) was observed during treatment, often anticipated by metabolic alterations such as onset of glucose intolerance, diabetes, hypercholesterolemia and hypertension. These effects have led to suspicion that TKIs may induce a chronic inflammatory response and it is necessary to understand which events are directly related to the drugs and which are mediated by other factors. In recent years, the study of the human microbiota has acquired increasing importance, thank to the great development of the omic sciences. Several evidences suggested that the gut microbiota regulates inflammation by affecting cytokine production and hematopoiesis, as well as by affecting the differentiation of inflammatory cell types. There is no literature on the interactions of gut microbiota with TKIs in CML. Given the plasticity in microbial composition and function, microbial-based therapeutic interventions, including dietary modulation, prebiotics and probiotics, potentially permit the development of novel strategies for CML therapy to improve clinical outcomes.
Research activity
My research unit aims to assess the role of IKB-alpha/NFkB in cancer and in particular hematological cancers. We also focus our efforts in the assessment on how cancer is associated with thrombosis development. My team is composed of an AIRC fellow, Dr. Giovanna Carrà, and a PhD student, Dr. Beatrice Maffeo.
Ongoing projects
Role of IkB-alpha in the modulation of mitochondria in cancer
Settore: Med/09
Ente finanziatore: Health Minister
Partecipanti al progetto: Dr. Giovanna Carrà, Dr Beatrice Maffeo
Abstract: We have recently described a novel role for IkB-alpha in the modulation of mitochondria in cancer. Using mass-spectrometry we have characterized the IkB-alpha interactome providing new clues on NF-kB independent functions for IkB-alpha
Determinant of thrombosis in cancers
Settore: Med/09
Ente finanziatore: ALT association
Partecipanti al progetto: Dr. Giovanna Carrà, Dr Beatrice Maffeo
Abstract: We aim to study how cancer is able to promote thrombosis.
Pubblicazioni
- Carrà G, Ermondi G, Riganti C, Righi L, Caron G, Menga A, Capelletto E, Maffeo B, Lingua MF, Fusella F, Volante M, Taulli R, Guerrasio A, Novello S, Brancaccio M, Piazza R, Morotti A. IκBα targeting promotes oxidative stress-dependent cell death. J Exp Clin Cancer Res. 2021 Apr 16;40(1):136. doi: 10.1186/s13046-021-01921-x
- Di Savino A, Panuzzo C, Rocca S, Familiari U, Piazza R, Crivellaro S, Carrà G, Ferretti R, Fusella F, Giugliano E, Camporeale A, Franco I, Miniscalco B, Cutrin JC, Turco E, Silengo L, Hirsch E, Rege-Cambrin G, Gambacorti-Passerini C, Pandolfi PP, Papotti M, Saglio G, Tarone G, Morotti A, Brancaccio M. Morgana acts as an oncosuppressor in chronic myeloid leukemia. Blood. 2015 Apr 2;125(14):2245-53.
- Morotti A, Panuzzo C, Crivellaro S, Pergolizzi B, Familiari U, Berger AH, Saglio G, Pandolfi PP. BCR-ABL disrupts PTEN nuclear-cytoplasmic shuttling through phosphorylation-dependent activation of HAUSP. 2014 Jun;28(6):1326-33.
- Barale C, Senkeev R, Napoli F, De Gobbi M, Guerrasio A, Morotti A, Russo I. Transferrin Saturation Inversely Correlates with Platelet Function. Thromb Haemost. 2019 May;119(5):766-778.
- Ito K, Bernardi R, Morotti A, Matsuoka S, Saglio G, Ikeda Y, Rosenblatt J, Avigan DE, Teruya-Feldstein J, Pandolfi PP. PML targeting eradicates quiescent leukaemia-initiating cells. Nature. 2008 Jun 19;453(7198):1072-8.